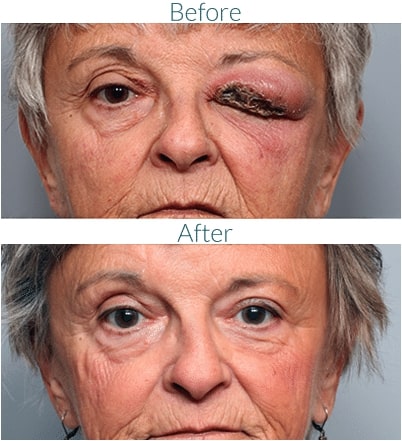
Orbital Cellulitis
Infections near the eye can occur just under the skin, or sometimes deeper in the tissues around the eye (or orbit). For children and adults, orbital infection is usually associated with sinus infections. When the infection occurs deep in the eye socket area, it can be dangerous, causing blindness and even death.

Certain conditions including diabetes increase the risk of serious infections, and blunt facial trauma will occasionally trigger severe infection. Prompt treatment with intravenous antibiotics is often necessary, sometimes combined with surgical drainage of the abscess.
Orbital Cellulitis Symptoms
- Protruding eye, also called proptosis
- Pain in or around the eye
- Nasal tenderness
- Swelling of the eye area
- Inflammation and redness
- Inability to open the eye
- Trouble moving the eye and pain upon movement of the eye
- Double vision
- Vision loss or impaired vision
- Discharge from the eye or nose
- Fever
- Headache

Causes of Orbital Cellulitis
Bacterial infections cause this condition, most commonly Streptococcus and Staphylococcus aureus (“staph”). This condition is more common in children. In children 9 and under, typically orbital cellulitis is caused by a single type of bacteria, but in older children and adults the infection can be caused by multiple strains simultaneously, which may make the condition more difficult to treat.
The vast majority of orbital cellulitis cases begin as untreated bacterial sinus infections that spread behind the orbital septum, or thin membrane separating the front part of the eye socket from the back portion of the eye socket.
Wounds, bug bites, animal bites, or even eyebrow waxing near the eye or eyebrow may also lead to orbital cellulitis, as can bacteria that have spread from a tooth infection.
Diagnosing Orbital Cellulitis
Orbital cellulitis can usually be diagnosed simply with an in-office examination of the patient’s eye. An examination can also determine if the infection is a similar condition that occurs in front of the orbital septum rather than behind it — preseptal cellulitis, which is less serious and will typically respond to oral antibiotics.
Additionally, these tests may be used for diagnosis:
- CT scan or MRI
- Physical examination of the nose, teeth, and mouth
- Cultures take from eye discharge, wound, or the nose
Orbital Cellulitis Treatment Options
Orbital cellulitis can be uncomfortable or painful, but the first treatment option isn’t necessarily surgery. Usually, antibiotics are the first treatment option. Depending on the severity of orbital cellulitis, the patient may require hospital admission in order to receive intravenous (IV) antibiotics. Broad-spectrum antibiotics are given due to the severity of this condition and the likelihood of multiple bacterial strains.
However, if antibiotics are not improving the condition, the next option is surgery to drain an abscess or fluid collection and obtain a culture sample for further microbial analysis.
Candidates for Orbital Cellulitis Surgery
Patients requiring surgery would find that his or her symptoms were not improving, or they may even have worsened despite the introduction of antibiotics. Surgery would then be necessary to stop the progression of the infection. Surgical intervention is more likely to be necessary for adults who have orbital cellulitis. These are other reasons a person could need this surgery:
- Worsening symptoms or vision impairment while taking antibiotics.
- A developing abscess in the eye socket or the brain.
- A foreign object trapped in the eye socket.
- A fungal or mycobacterial infection.
What Happens if Orbital Cellulitis is Left Untreated?
This is a serious condition that requires early diagnosis and treatment. If orbital cellulitis is left untreated, it can progress to the point of causing blindness or becoming life-threatening. Without treatment, various complications can develop, such as:
- Vision loss
- Hearing loss
- Blood infection (sepsis)
- Meningitis, inflammation of the linings of the brain and spinal cord
- Cavernous sinus thrombosis, the formation of a blood clot at the base of the brain
- Intracranial abscess, an accumulation of pus inside the skull
Read What Our Patients Are Saying!
"Very professional and honest. The best injector I’ve ever had! I love my results and I will forever be his client. The staff was very warm and made my experience very nice and comfortable."
Click here to read more reviews.
Schedule a Consultation
If you are experiencing symptoms of orbital cellulitis, contact our Denver office today! Call 303-839-1616 to schedule a consultation with facial plastic surgeon Dr. Robert Fante.