Industry Leading Graves Disease Treatment in Co
This year has had a mix of good and bad news, but we had some great news regarding the medical treatment of thyroid eye disease with Tepezza® (teprotumumab). Tepezza® is a monoclonal antibody that was newly approved by the FDA in January 2020 for the treatment of thyroid eye disease after highly successful clinical trials. Nothing works for everyone, but Tepezza® improves eye bulging, double vision, and eye inflammation for the majority of people treated. Treatment consists of eight intravenous infusions over 6 months. Dr. Fante are among the first specialists using Tepezza® in Colorado and have lectured to other physicians about it. Make an appointment today to see if you are a candidate!
What is Graves Disease?
The autoimmune thyroid-related disease can cause a wide range of symptoms and problems for the eyes, including bulging, redness, tearing, irritation, double vision, pain, pressure, and rarely, loss of vision. The eye problems can start before, after, or during the thyroid problem, and typically progress slowly over about 18-30 months. For a minority of people, the problems are minor and completely resolve, but for most people, the discomfort and change in appearance are long-lasting.
Causes of Graves Disease
Thyroid eye disease (also known as Graves’ disease) is an autoimmune disease in which a person’s immune system mistakenly begins to ‘attack’ the thyroid gland and the tissues around the eyes. Cells in both of these areas have protein on their surface (called an antigen) in common, and the immune system begins making antibodies against this protein.
This will then initiate inflammation that causes redness & swelling, loss of function, and scarring. The exact cause isn’t yet known, but we do know that thyroid eye disease is more common in women and in people with other autoimmune diseases including celiac disease, autoimmune gastritis, and myasthenia gravis. Not everyone has problems with both the thyroid gland and the eyes, but there is research evidence that removal of the thyroid gland may be protective for the eyes.

About 50% of people who have graves disease will develop eye disease, while about 90% of people will be hyperthyroid if they have eye disease.
Thyroid Eye Disease Symptoms
Thyroid eye disease has many symptoms which can vary a great deal among different people.
- The most common are:
- Tearing, burning, redness and drying of the eyes
- Increased sensitivity to light
- Swelling of the eyelids
- Achy pain or pressure behind the eyes
- Bulging of one or both eyes (this is usually first noticed in photographs)
Less common symptoms are:
- Redness and thickening of the skin around the eyes, eyebrows, and cheeks
- Double vision
Double vision can occur intermittently, or only when looking in certain directions, or all of the time. This is a little scarier than the other symptoms above because it affects visual function more profoundly. Even less common (and scarier) than double vision is loss of vision, which occurs in less than 1% of people with thyroid eye disease, and can start as a greying or loss of color vision in one eye. Because the loss of vision is an emergency typically requiring urgent treatment, it is important to see an eye doctor if you experience any group of the symptoms above.
Thyroid Disease Symptoms
Since many people with thyroid eye disease also have thyroid disease itself, we should review some of those symptoms too. Most people with new-onset of Graves’ disease will have hyperthyroidism, which means that their thyroid gland is producing too much thyroid hormone. Common symptoms of hyperthyroidism include anxiety, tremor, rapid heartbeat, unexplained weight loss, intolerance to heat, change in menstrual pattern, and swelling in the neck.
Dr. Fante has lectured extensively on Thyroid Eye Disease, and his recent lecture “Thyroid Eye Disease: the State of the Art, and What We Still Don’t Know” was published nationally by the Audio-Digest, an audio magazine for continuing physician education.
Listen to Dr. Fante discuss Thyroid Disease
Diagnosing Graves Disease
To test for Graves’s Disease, a specialist will listen carefully to the person’s symptoms, examine the person, and then evaluate blood tests and imaging studies to make the diagnosis of thyroid eye disease. The blood tests usually include thyroid hormone function tests, and also a measurement of the antibody against the thyroid receptor that is common to the eye area and the thyroid.
This is called the TSH receptor antibody and the test is usually called TSI (for thyroid-stimulating immunoglobulin). It is not a perfect test, but higher values generally follow more severe disease, and a value above 400 is at higher risk. Finally, common imaging studies will typically include CT scans and MRI scans of the eye area (called the orbit) that will typically show thickening of the eye muscles and/or fat around the eye. Imaging is also helpful to show that there isn’t something else (such as a tumor) causing the person’s symptoms.

Graves Disease Treatment Options
Overall, only about half of the people with Graves’ hyperthyroid disease will develop the related eye disease. Research has shown that several things are protective and will make it less likely that a person with the thyroid disease will get the eye disease too. Not smoking is the first of these – people with Graves’ should not smoke. Also, recent research indicates that statins (drugs usually prescribed for their cholesterol-lowering effect) may be protective. Finally, there is evidence that surgical removal of the thyroid gland may be protective.
There are several options for treatment of the excessive thyroid hormone in people with Graves’ hyperthyroidism and these include surgical removal of the thyroid gland, ablation (destruction) of the thyroid gland with radioactive iodine, as well as the use of pills that suppress thyroid hormone production. Each of these surgeries has advantages and disadvantages and should be discussed with a qualified medical professional such as an endocrinologist.
Treatment for the eye disease is typically initiated during the active phase while inflammation is evident, and sometimes involves oral and intravenous medications, radiation, eye drops, ointments, and prism glasses. Dr. Fante are one of the few Colorado specialists who commonly treat this disease. Treatment is then coordinated with primary care physicians or endocrinologists as needed. Also, it is important to note that tobacco use is very harmful in this disease and patients are admonished to stop smoking.
Thyroid Eye Disease Treatment Before and After
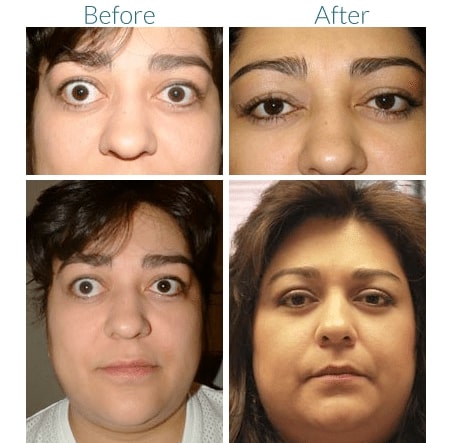
Reconstructive Eye Treatment for Graves Disease
For many patients, reconstructive surgery is very helpful in restoring normal function and appearance to the eyes. There are three possible phases of rehabilitative surgery used as needed: orbital decompression to reduce eye-bulging, eye muscle surgery to reduce double vision, and eyelid surgery to restore normal size and shape. Although most patients do not need all of these phases, and many need no surgery at all.

"As I expressed in my Google review (Franci Greenberg) I could not be more grateful for Dr. Fante and his staff. He is BY FAR the best doctor I think I will EVER have in my lifetime. Thank you so very much!"
Recovery After Thyroid Eye Disease Treatment
Since most surgical procedures that are performed in an operating room will cause swelling and bruising, you will have sutures that require care for the first week or two. During this period, you’ll be able to see, move about, and accomplish a lot, but you will probably have at least one “black” eye. You will then be asked to avoid strenuous activities for the first week or two, and if necessary, you will be given more specific instructions on travel, bathing, and post-op care.
Your healing will be dependent on which procedure you are having done, your compliance with pre- and post-operative instructions, and your overall health. In addition, we will do our very best to make sure that you have all the information you and your caregivers will need to provide the best care possible. We are always here to help and available if any questions or concerns arise.
Schedule a Consultation
If you are interested in treatment for Graves Disease, contact our office today! Call 303-839-1616 to schedule a consultation with Denver Facial Plastic Surgery Dr. Robert Fante.